Functional Medicine for Autoimmune Disorders: Root Cause Solutions
Your doctor tells you that your autoimmune condition is "just something you'll have to live with" while prescribing another immunosuppressive medication to manage your symptoms. Meanwhile, your fatigue worsens, joint pain persists, and digestive issues continue to disrupt your daily life. This scenario unfolds in countless medical offices daily, leaving millions feeling hopeless about conditions like Hashimoto's thyroiditis, rheumatoid arthritis, and lupus. Recent advances in functional medicine reveal that autoimmune disorders often stem from identifiable root causes, particularly gut dysfunction, chronic stress, and nutrient deficiencies, that can be addressed through targeted interventions rather than lifelong symptom suppression.
This systems-based approach offers hope for lasting improvements by addressing the underlying mechanisms driving autoimmune inflammation rather than simply masking the consequences.
The Gut-Immune Connection: Where Autoimmunity Begins
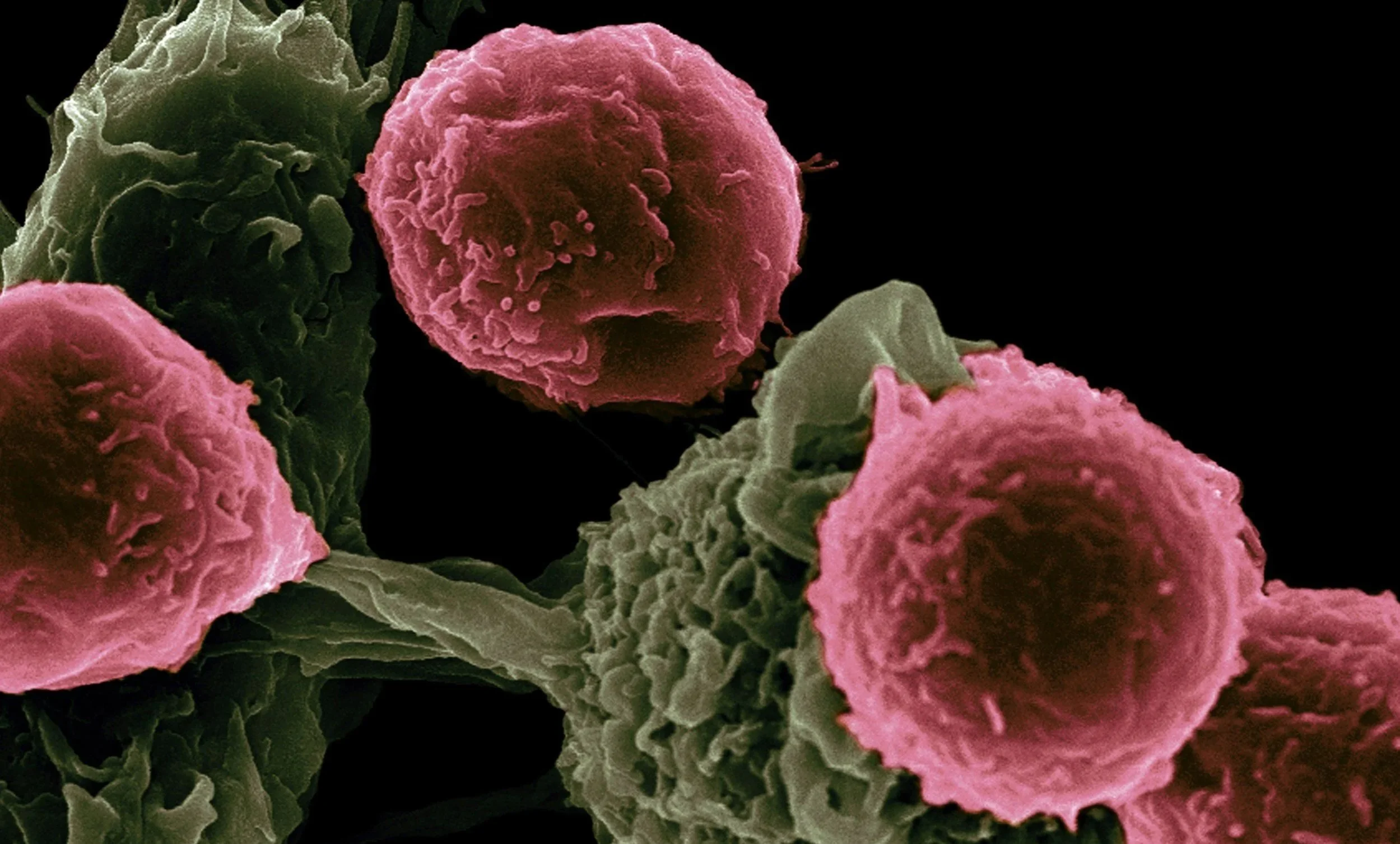
Your intestinal tract houses approximately 70% of your immune system, making gut health fundamental to immune balance. The intestinal barrier serves as the body's first line of defense, selectively allowing nutrients to pass while blocking harmful substances. When this barrier becomes compromised (a condition known as intestinal permeability, or "leaky gut") bacterial fragments, undigested food particles, and toxins can trigger inappropriate immune responses.
Recent research demonstrates that psychological stress significantly impairs intestinal barrier function through multiple pathways. Chronic stress elevates cortisol levels, which disrupts tight junction proteins that maintain intestinal integrity. Stress also alters the gut microbiome composition, reducing beneficial bacteria while promoting pathogenic species that further damage the intestinal lining. This creates a cascading effect where stress-induced gut dysfunction triggers systemic inflammation that can initiate or exacerbate autoimmune conditions.
The gut microbiome plays a crucial role in training and regulating immune responses. Beneficial bacteria produce short-chain fatty acids like butyrate, which support regulatory T cells that prevent excessive immune activation. When dysbiosis occurs, characterized by reduced microbial diversity and overgrowth of potentially harmful species, this protective mechanism fails. Studies show that patients with autoimmune disorders consistently exhibit distinct microbiome signatures with reduced beneficial strains and increased inflammatory species.
Molecular mimicry represents another critical mechanism linking gut dysfunction to autoimmunity. When intestinal permeability allows bacterial fragments to enter systemic circulation, the immune system may create antibodies against these foreign proteins. If these bacterial proteins share structural similarities with human tissues, the resulting antibodies can cross-react with the body's own cells, triggering autoimmune attacks. This explains why certain bacterial infections often precede autoimmune disease onset.
Nutritional Strategies for Specific Autoimmune Conditions
Functional medicine recognizes that different autoimmune conditions benefit from targeted nutritional interventions based on their unique pathophysiology and triggers. While all autoimmune disorders share common inflammatory pathways, each condition has specific nutritional needs and sensitivities that must be addressed for optimal outcomes. Let's walk through a few of them below.
Hashimoto's Thyroiditis: Supporting Thyroid Function and Reducing Inflammation
Hashimoto's thyroiditis, the most common cause of hypothyroidism, involves immune-mediated destruction of thyroid tissue. Nutritional interventions focus on reducing thyroid antibodies, supporting hormone conversion, and addressing nutrient deficiencies that impair thyroid function.
Selenium plays a critical role in thyroid hormone metabolism and immune regulation. Studies demonstrate that selenium supplementation can significantly reduce thyroid peroxidase antibodies and improve thyroid function in Hashimoto's patients. The optimal dose appears to be 200 micrograms daily, though individual needs may vary based on baseline selenium status.
Iodine presents a complex consideration in Hashimoto's management. While essential for thyroid hormone synthesis, excessive iodine can trigger autoimmune flares in susceptible individuals. Functional medicine practitioners typically assess iodine status through comprehensive testing and implement cautious supplementation protocols when deficiency is confirmed.
Gluten elimination proves beneficial for many Hashimoto's patients due to molecular mimicry between gluten proteins and thyroid tissue. Research shows that gluten-sensitive individuals with Hashimoto's often experience reduced antibody levels and improved symptoms when following a strict gluten-free diet. This intervention requires complete elimination rather than mere reduction, as even small amounts can trigger immune reactions.
Anti-inflammatory nutrients like omega-3 fatty acids, curcumin, and vitamin D help modulate the autoimmune response. Omega-3s from fish oil reduce inflammatory cytokines while supporting regulatory T cell function. Curcumin inhibits nuclear factor-kappa B, a key inflammatory pathway involved in autoimmune progression.
Rheumatoid Arthritis: Targeting Joint Inflammation and Systemic Immunity
Rheumatoid arthritis involves chronic inflammation of synovial joints, driven by complex interactions between genetic susceptibility, environmental triggers, and immune dysregulation. Nutritional interventions aim to reduce inflammatory cytokines, support joint tissue repair, and modulate immune function.
The gut microbiome plays a particularly important role in rheumatoid arthritis. Research identifies specific bacterial strains that can trigger inflammatory responses leading to joint inflammation. Prevotella copri, for example, is overrepresented in many RA patients and appears to promote inflammatory T helper 17 cell responses. Conversely, beneficial bacteria like Lactobacillus species help maintain immune tolerance and reduce inflammatory cytokine production.
Omega-3 fatty acids demonstrate remarkable efficacy in reducing RA symptoms and disease progression. EPA and DHA compete with arachidonic acid for enzyme systems, shifting eicosanoid production from inflammatory to anti-inflammatory compounds. Clinical trials show that fish oil supplementation can reduce joint tenderness, morning stiffness, and the need for anti-inflammatory medications.
Elimination diets prove valuable for identifying food triggers that exacerbate RA symptoms. Common culprits include nightshade vegetables (tomatoes, potatoes, peppers, eggplant), dairy products, and processed foods high in advanced glycation end products. The autoimmune protocol (AIP) diet provides a structured approach to identifying these triggers through systematic elimination and reintroduction.
Antioxidant compounds help combat the oxidative stress that contributes to joint destruction in RA. Quercetin inhibits inflammatory enzymes while stabilizing mast cells. Green tea polyphenols reduce inflammatory cytokines and may slow cartilage degradation. Tart cherry extract provides natural anti-inflammatory compounds that can reduce pain and improve sleep quality.
Lupus: Modulating Immune Complexity and Organ Protection
Systemic lupus erythematosus involves widespread immune dysfunction affecting multiple organ systems. Nutritional strategies focus on immune modulation, reducing inflammatory burden, and protecting vulnerable organs like the kidneys and cardiovascular system.
Vitamin D deficiency is extremely common in lupus patients and contributes to disease severity. Vitamin D acts as an immune modulator, promoting regulatory T cells while suppressing inflammatory cytokine production. Many lupus patients require higher doses than typically recommended, often 4,000-6,000 IU daily, to achieve optimal blood levels.
N-acetylcysteine (NAC) shows promise in lupus management through multiple mechanisms. NAC replenishes glutathione, the body's primary antioxidant defense system, which is typically depleted in lupus patients. It also modulates T cell function and may reduce autoantibody production. Clinical studies demonstrate that NAC supplementation can improve fatigue, reduce disease activity, and protect kidney function.
Resveratrol and other polyphenolic compounds help regulate the interferon pathways that are overactive in lupus. These compounds can reduce type I interferon signaling, which drives much of the inflammation and tissue damage in lupus. Turmeric, green tea, and grape seed extract all contain beneficial polyphenols with immune-modulating properties.
The Mediterranean diet pattern consistently shows benefits for lupus patients, likely due to its anti-inflammatory profile and microbiome-supporting properties. This eating pattern emphasizes omega-3 rich fish, antioxidant-dense vegetables, healthy fats from olive oil and nuts, and fiber-rich legumes while limiting processed foods and excess sugar.
The Stress-Autoimmune Connection
Chronic stress acts as both a trigger and perpetuator of autoimmune disorders through complex neuroendocrine and immune pathways. Understanding and addressing stress is crucial for achieving lasting improvements in autoimmune conditions.
Psychological stress disrupts the hypothalamic-pituitary-adrenal (HPA) axis, leading to dysregulated cortisol production. While acute cortisol elevation can be immunosuppressive, chronic stress often results in cortisol resistance, where tissues become less responsive to cortisol's anti-inflammatory effects. This creates a state of ongoing inflammation that can trigger or worsen autoimmune responses.
Stress directly impacts gut barrier function through multiple mechanisms. The enteric nervous system, often called the "second brain," responds to psychological stress by altering intestinal permeability and motility. Stress hormones like corticotropin-releasing hormone increase mast cell activation in the gut, leading to inflammatory mediator release and barrier dysfunction. This stress-induced intestinal permeability allows bacterial translocation that can trigger systemic autoimmune responses.
The timing of stress exposure influences its impact on autoimmune development. Early life stress, including childhood trauma, appears particularly damaging to immune development and increases autoimmune risk in adulthood. This may occur through epigenetic modifications that alter immune gene expression throughout life. Adult stress exposure more commonly triggers flares in existing autoimmune conditions rather than initiating new disease.
Effective stress management requires addressing both the physiological and psychological aspects of the stress response. Adaptogenic herbs like ashwagandha, rhodiola, and holy basil help modulate cortisol production and improve stress resilience. These botanicals support healthy HPA axis function while reducing inflammatory cytokine production.
Mind-body practices prove particularly effective for autoimmune patients. Meditation, yoga, and tai chi activate the parasympathetic nervous system while reducing inflammatory markers. Research shows that regular meditation practice can reduce disease activity in rheumatoid arthritis and improve quality of life in lupus patients. The key lies in consistency rather than duration, where even just 10-15 minutes of daily practice can produce measurable benefits.
Sleep optimization also deserves special attention, as sleep disturbances both contribute to and result from autoimmune inflammation. Poor sleep quality increases inflammatory cytokines while impairing immune regulation. Creating consistent sleep schedules, optimizing the sleep environment, and addressing underlying sleep disorders like sleep apnea can significantly improve autoimmune symptoms.
Dr. Holtski's Comprehensive Approach to Autoimmune Care
At Brighter Balance, I utilize the full breadth and naturopathic and functional medicine principles to address the root causes of autoimmune disorders through personalized, evidence-based interventions. My approach begins with comprehensive assessment including detailed symptom tracking, environmental exposure history, stress evaluation, and specialized laboratory testing that goes far beyond conventional autoimmune panels. Depending on each individual's concerns, this may include tests like a comprehensive stool analysis to assess microbiome composition and gut barrier function, food sensitivity testing to identify dietary triggers, advanced nutrient analysis to detect deficiencies that contribute to immune dysfunction, organic acid testing to reveal metabolic imbalances, toxic burden assessment identifies environmental factors that may be perpetuating autoimmune responses, and much more.
Based on these findings, I develop personalized treatment protocols that integrate targeted nutrition plans, strategic supplementation, gut healing interventions, and stress management techniques. This often includes elimination diets tailored to individual sensitivities, specific probiotic strains chosen based on microbiome analysis, and botanicals selected for their immune-modulating properties.
My treatment plans evolve based on patient response and follow-up testing, ensuring optimal outcomes while minimizing adverse effects. Many patients experience significant improvements in energy, pain levels, and overall quality of life within months of beginning comprehensive functional medicine protocols. When appropriate, I also coordinate care with conventional specialists to ensure patients receive integrated treatment that addresses both immediate symptom management and long-term healing.
The functional medicine approach recognizes that autoimmune recovery often requires months to years of consistent intervention, as the immune system gradually rebalances and tissues repair. I provide ongoing support and education throughout this process, empowering patients to understand their conditions and take active roles in their healing journeys. Whenever you're ready to address the root causes of your autoimmune condition rather than merely managing symptoms, I'm here to offer evidence-based solutions that target the underlying mechanisms driving autoimmune inflammation, providing hope for lasting improvements in health and quality of life. Schedule your comprehensive consultation today on our Scheduling Page.
References and Further Reading:
“Gut Microbiota, Leaky Gut, and Autoimmune Diseases” https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.946248/full
“The Gut-Brain Axis in Autoimmune Diseases: Emerging Insights and Therapeutic Implications” https://assets.cureus.com/uploads/review_article/pdf/194950/20231211-6994-q64bwf.pdf
“Psychological Stress, Intestinal Barrier Dysfunctions, and Autoimmune Disorders: An Overview” https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01823/full